Imagine facing an infection that just won't back down. When standard antibiotics falter, particularly against stubborn Gram-negative bacteria, medical professionals often turn to a powerful class of drugs: Key Third-Generation Cephalosporin Drugs and Examples. These aren't just any antibiotics; they're a cornerstone of modern infectious disease treatment, offering a critical defense line where earlier options might fail.
From everyday practice to life-threatening scenarios, understanding these medications is vital for patients, caregivers, and healthcare professionals alike. They represent a significant leap forward in antibiotic development, giving us more sophisticated tools to combat a wide spectrum of bacterial threats.
At a Glance: Third-Generation Cephalosporins
- What they are: A class of broad-spectrum antibiotics effective against many bacterial infections, especially Gram-negative strains.
- How they work: They kill bacteria by disrupting their cell wall formation.
- Key uses: Treat serious infections like sepsis, meningitis, pneumonia, UTIs, skin infections, and more.
- Major players: Includes drugs like ceftriaxone, cefotaxime, ceftazidime, cefixime, and cefdinir.
- Special features: Some offer anti-pseudomonal activity, others penetrate the brain (CNS), and some have convenient once-daily dosing.
- Important considerations: Generally safe but can cause allergic reactions (cross-reactivity with penicillin allergy), digestive issues, and in rare cases, more serious side effects. Always take exactly as prescribed.
The Science Behind the Shield: How Third-Generation Cephalosporins Work
Think of bacteria as tiny fortresses, protected by a sturdy outer wall. For bacteria to survive and multiply, they constantly need to build and repair this cell wall. This is where Explore third-generation cephalosporins come in, acting as precision demolition experts.
Derived from the Acremonium mold, these antibiotics belong to the broader family of beta-lactam antibiotics. Their secret weapon is a unique beta-lactam ring structure. This ring is designed to mimic a crucial building block that bacteria use to construct their cell walls. When a third-generation cephalosporin enters a bacterial cell, it binds irreversibly to specific enzymes called penicillin-binding proteins (PBPs). These PBPs are like the construction workers responsible for cross-linking peptidoglycans, the essential scaffolding of the bacterial cell wall.
By blocking these PBPs, the antibiotic effectively stops the construction process. The bacterial cell wall becomes weak, leaky, and eventually, the cell can no longer maintain its structural integrity. It ruptures and dies – a bactericidal effect. This direct bacterial killing power is why these drugs are so effective in treating serious infections.
Why the "Third Generation" Matters: Evolving Against Resistance
Cephalosporins aren't a monolithic group. They're divided into five generations, each designed to tackle a progressively wider range of bacteria and overcome resistance patterns that might render older generations ineffective. The third generation represents a significant leap for several key reasons:
- Enhanced Gram-Negative Coverage: While earlier generations had some Gram-negative activity, third-gen cephalosporins are specifically engineered to be much more potent against a broader spectrum of these difficult-to-treat bacteria, including many strains of Enterobacteriaceae. This is crucial because Gram-negative bacteria are often responsible for serious infections like sepsis, pneumonia, and UTIs, and they're notorious for developing resistance.
- Improved Resistance Profile: They were developed to be more resistant to destruction by beta-lactamase enzymes, which are bacterial defenses that break down older beta-lactam antibiotics. This doesn't mean they're invulnerable, but they offer a stronger fighting chance.
- Central Nervous System (CNS) Penetration: Many third-generation cephalosporins have the unique ability to cross the blood-brain barrier, making them invaluable for treating infections within the brain and spinal cord, such as meningitis.
In essence, the development of third-generation cephalosporins was a strategic move in the ongoing battle against bacterial infections, arming healthcare providers with more potent and versatile weapons.
The Frontline Players: Key Third-Generation Cephalosporin Drugs and Examples
When we talk about specific third-generation cephalosporins, it's important to understand that while they share common characteristics, each drug has its own nuances, making them suitable for different clinical situations. Here’s a closer look at some of the most important ones:
The Intravenous/Intramuscular Powerhouses
These are typically used for more severe infections requiring hospitalization or strong initial treatment.
- Ceftriaxone (Rocephin):
- The Go-To: Often considered the most commonly used third-generation cephalosporin worldwide. Its long half-life allows for convenient once-daily dosing, which is a major advantage for both patients and healthcare providers.
- Key Strengths: Excellent activity against many Gram-negative bacteria (including Haemophilus influenzae, Neisseria gonorrhoeae, and most Enterobacteriaceae), and good Gram-positive coverage (e.g., Streptococcus pneumoniae). It also penetrates the cerebrospinal fluid effectively.
- Common Uses: Widely used for community-acquired pneumonia, bacterial meningitis, complicated urinary tract infections, skin and soft tissue infections, bone and joint infections, intra-abdominal infections, sepsis, and is a first-line treatment for gonorrhea and pelvic inflammatory disease.
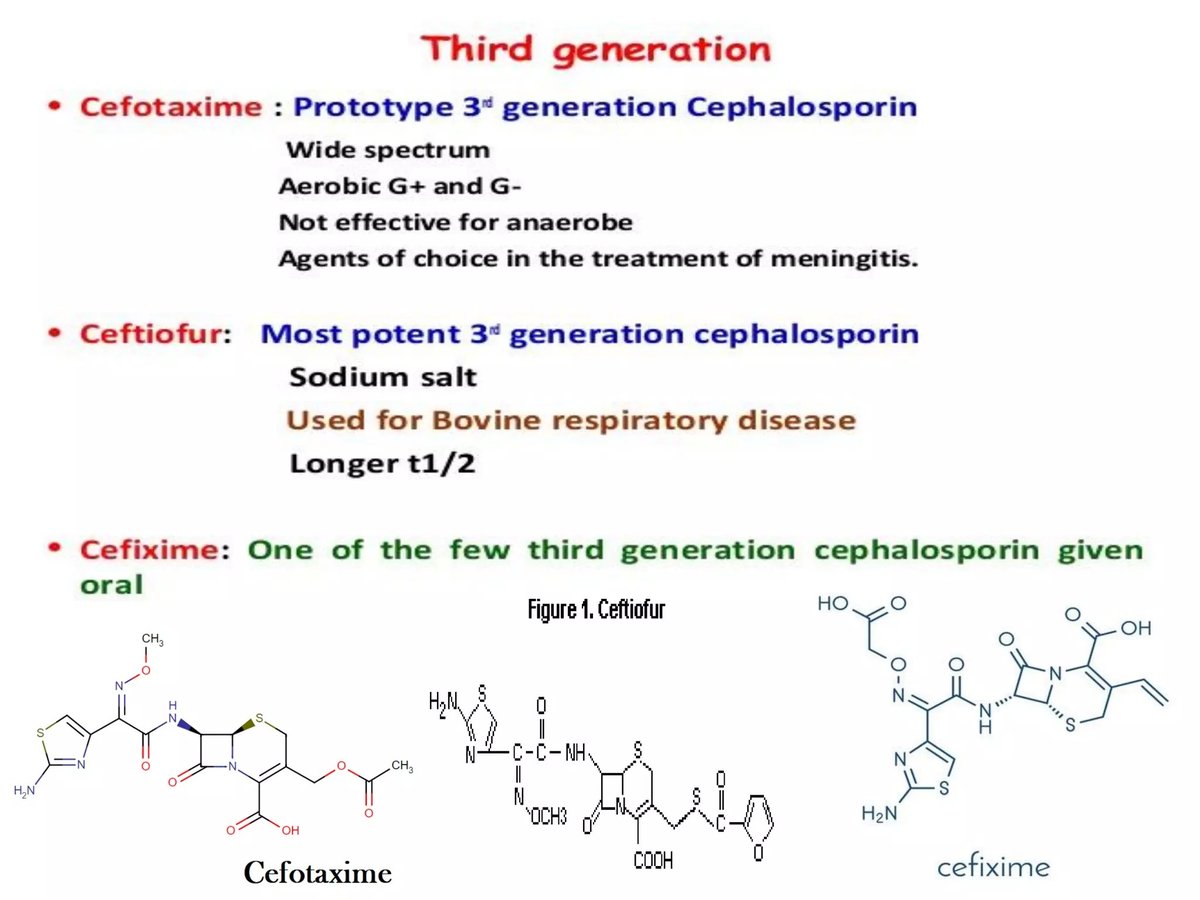
- Cefotaxime (Claforan):
- A Close Relative: Shares many similarities with ceftriaxone, including good Gram-negative and Gram-positive coverage, and excellent CNS penetration.
- Key Strengths: Particularly noted for its strong Gram-positive coverage among the third-gens, alongside good Gram-negative activity.
- Common Uses: Frequently used for bacterial meningitis, neonatal sepsis, serious lower respiratory tract infections, and other severe infections. It's often chosen for neonates due to ceftriaxone's risk of bilirubin displacement in infants.
- Important Note: Rapid bolus administration of cefotaxime has been rarely associated with potentially life-threatening arrhythmias, underscoring the importance of correct administration.
- Ceftazidime (Fortaz, Tazicef):
- The Antipseudomonal Specialist: This is where ceftazidime truly stands out. Unlike ceftriaxone and cefotaxime, ceftazidime offers potent activity against Pseudomonas aeruginosa, a particularly challenging Gram-negative bacterium often associated with hospital-acquired infections in immunocompromised patients or those with cystic fibrosis.
- Key Strengths: Excellent Gram-negative coverage, including Pseudomonas.
- Common Uses: Crucial for treating severe Pseudomonas infections, hospital-acquired pneumonia, ventilator-associated pneumonia, febrile neutropenia, and complicated UTIs where Pseudomonas is suspected.
- Caveat: Its Gram-positive coverage is generally weaker compared to ceftriaxone or cefotaxime.
- Ceftazidime/Avibactam (Avycaz):
- A Modern Combination: This isn't just a third-gen cephalosporin; it's a potent combination of ceftazidime with avibactam, a beta-lactamase inhibitor.
- Key Strengths: Avibactam protects ceftazidime from destruction by a wider range of bacterial beta-lactamase enzymes, including some carbapenemases (KPC, OXA-48), which are responsible for very difficult-to-treat resistance. This significantly broadens ceftazidime's activity against highly resistant Gram-negative bacteria.
- Common Uses: Reserved for serious infections caused by multidrug-resistant Gram-negative bacteria, such as complicated intra-abdominal infections, complicated urinary tract infections, and hospital-acquired/ventilator-associated pneumonia when other options have failed.
The Oral Options: Convenience for Less Severe Cases
While the intravenous forms tackle the toughest infections, several third-generation cephalosporins are available in oral formulations, making them suitable for outpatient treatment or stepping down from IV therapy once a patient is stable.
- Cefixime (Suprax):
- Oral Workhorse: One of the most common oral third-generation cephalosporins.
- Key Strengths: Good activity against many Gram-negative bacteria, including Haemophilus influenzae, Moraxella catarrhalis, and Streptococcus pneumoniae. Also effective against N. gonorrhoeae.
- Common Uses: Used for uncomplicated urinary tract infections, otitis media (ear infections), pharyngitis/tonsillitis, acute bronchitis, and uncomplicated gonorrhea.
- Cefdinir (Omnicef):
- Broad-Spectrum Oral: Another popular oral option with a broad spectrum of activity.
- Key Strengths: Effective against a similar range of bacteria as cefixime, including common respiratory pathogens and Gram-positive cocci.
- Common Uses: Widely prescribed for community-acquired pneumonia, acute exacerbations of chronic bronchitis, sinusitis, pharyngitis/tonsillitis, skin and soft tissue infections, and uncomplicated UTIs.
- Cefpodoxime (Vantin):
- Similar Profile: Offers a similar spectrum of activity to cefixime and cefdinir.
- Key Strengths: Good coverage against many common respiratory tract pathogens and Gram-negative bacteria.
- Common Uses: Treats a variety of mild to moderate infections including acute otitis media, pharyngitis/tonsillitis, community-acquired pneumonia, acute bronchitis, and uncomplicated urinary tract infections.
Historical & Discontinued Examples
Some third-generation cephalosporins, while no longer widely available, were significant in their time and help illustrate the evolution of the class:
- Ceftizoxime (Cefizox): Offered good Gram-positive coverage, similar to cefotaxime.
- Cefoperazone (Cefobid, Spectracef): Notable for its antipseudomonal activity, similar to ceftazidime, but it did not penetrate the cerebrospinal fluid, limiting its use for CNS infections.
- Cefditoren (Spectracef): An oral option.
- Ceftibuten (Cedax): Another oral option.
Even as some drugs are discontinued, their properties often inform the development and understanding of newer agents.
Where These Drugs Make a Difference: Common Applications
The broad spectrum and unique properties of third-generation cephalosporins make them invaluable for treating a diverse array of bacterial infections. Here’s a breakdown of common scenarios where you might encounter them:
- Bacteremia/Septicemia (Sepsis): When bacteria enter the bloodstream, leading to a life-threatening systemic inflammatory response, these drugs are often a first-line choice, especially ceftriaxone or cefotaxime, due to their broad coverage and efficacy.
- Central Nervous System Infections: Conditions like bacterial meningitis, where bacteria infect the membranes surrounding the brain and spinal cord, demand drugs that can cross the blood-brain barrier. Ceftriaxone and cefotaxime are workhorses here.
- Lower Respiratory Tract Infections: This includes severe cases of community-acquired pneumonia (CAP), hospital-acquired pneumonia (HAP), and ventilator-associated pneumonia (VAP). Ceftriaxone, cefotaxime, and especially ceftazidime (if Pseudomonas is suspected) are crucial.
- Urinary Tract Infections (UTIs): For complicated UTIs, pyelonephritis (kidney infection), or UTIs caused by resistant organisms, these cephalosporins (both IV and oral forms) are frequently used.
- Intra-abdominal Infections: These can range from appendicitis to diverticulitis or peritonitis. Often, they are used in combination with other antibiotics to cover a wider spectrum of bacteria, including anaerobes.
- Skin and Skin Structure/Soft Tissue Infections: For serious infections like cellulitis, erysipelas, or wound infections, particularly those acquired in healthcare settings or involving resistant organisms.
- Bone and Joint Infections: Osteomyelitis (bone infection) and septic arthritis often require prolonged courses of potent antibiotics, and third-generation cephalosporins are a common choice.
- Gynecological Infections: Including pelvic inflammatory disease (PID) and endometritis, where ceftriaxone is often a key component of treatment.
- Gonorrhea: Ceftriaxone is a cornerstone treatment for uncomplicated gonorrhea, often given in combination with another antibiotic to cover potential co-infections.
Administering These Powerful Drugs: What You Should Know
Third-generation cephalosporins can be administered in several ways, depending on the specific drug, the severity of the infection, and patient needs:
- Intravenously (IV): For serious infections requiring rapid and high concentrations of the antibiotic in the bloodstream. This is typical for hospitalized patients.
- Intramuscularly (IM): For certain infections (like gonorrhea) or when IV access isn't practical, some drugs like ceftriaxone can be given as an injection into a muscle.
- Orally: For less severe infections, or as a "step-down" therapy after initial IV treatment, several oral forms (like cefixime, cefdinir, cefpodoxime) are available.
Regardless of the route, it is absolutely paramount that these drugs are administered exactly as directed by a healthcare professional. This includes the correct dosage, frequency, and duration. Skipping doses or stopping treatment early can lead to treatment failure and contribute to antibiotic resistance.
Understanding the Risks: Potential Side Effects and Warnings
While third-generation cephalosporins are generally considered safe and well-tolerated with low toxicity, like all medications, they carry potential risks and side effects. Being aware of these is crucial for safe treatment.
Common Side Effects:
These are usually mild and manageable:
- Gastrointestinal Distress: Abdominal pain, nausea, vomiting, and diarrhea are fairly common.
- Injection Site Reactions: Pain, inflammation, or redness at the site of injection.
- Skin Reactions: Rash, or itchy skin.
- Transient Lab Changes: Temporary increases in liver enzymes (AST, ALT), or mild changes in blood counts (leukopenia, thrombocytopenia).
- Decreased Appetite: A general feeling of not wanting to eat.
Serious Side Effects & Warnings:
These are rarer but require immediate medical attention:
- Allergic Reactions: Ranging from mild rashes and hives to severe swelling (angioedema) or life-threatening anaphylaxis.
- Penicillin Allergy Cross-Reactivity: It's important to note that individuals with a penicillin allergy have about a 5-10% chance of also reacting to cephalosporins. Always inform your doctor if you have any drug allergies.
- Clostridium difficile Infection (CDI): Antibiotics can disrupt the natural balance of gut bacteria, allowing C. difficile to overgrow. This can cause severe, persistent diarrhea, abdominal pain, and in serious cases, pseudomembranous colitis. Seek immediate medical attention if you develop severe diarrhea during or after antibiotic treatment.
- Drug-Induced Immune Hemolytic Anemia (DIIHA): A rare but serious condition where the drug causes the immune system to mistakenly attack and destroy red blood cells, leading to anemia.
- Seizures: While rare, seizures can occur, particularly in individuals with pre-existing kidney disease, as the drug may accumulate to toxic levels. Dosage adjustments are critical in these patients.
- Bleeding Issues: Some cephalosporins can suppress gut flora, which are responsible for synthesizing vitamin K. Reduced vitamin K can interfere with blood clotting, potentially leading to increased bleeding. This is particularly relevant for those on blood thinners.
- Disulfiram-like Reactions: Rarely, some cephalosporins (like cefoperazone, though now discontinued) can cause a reaction similar to that experienced when alcohol is consumed while taking Disulfiram, leading to nausea, vomiting, flushing, and headache.
- Cardiac Arrhythmias: As noted, rapid bolus administration of cefotaxime has been reported to cause potentially life-threatening heart rhythm disturbances.
Always discuss your full medical history, including all allergies and other medications you are taking, with your healthcare provider before starting a third-generation cephalosporin.
Navigating Treatment: Practical Guidance for Patients and Caregivers
Understanding the medical jargon around antibiotics can feel overwhelming, but a few practical tips can empower you to be a more informed participant in your healthcare journey:
- Complete the Full Course: Even if you start feeling better, finish all prescribed doses. Stopping early can allow surviving bacteria to regrow and develop resistance.
- Report Side Effects Promptly: Don't hesitate to inform your doctor or pharmacist about any side effects you experience, especially severe diarrhea, rash, or breathing difficulties.
- Hydration is Key: Especially if you experience diarrhea or nausea, staying well-hydrated is important.
- Avoid Self-Medication: Never use leftover antibiotics or antibiotics prescribed for someone else. This is dangerous and contributes to antibiotic resistance.
- Ask Questions: If you're unsure about anything—dosage, timing, potential interactions with other medications, or what to expect—ask your healthcare provider or pharmacist. They are your best resource.
- Manage Expectations: While powerful, no antibiotic is a magic bullet. Recovery takes time, and consistent adherence to your treatment plan is crucial for the best outcome.
Your Role in the Fight Against Resistance
Third-generation cephalosporins are powerful tools, but their effectiveness depends on responsible use. The global rise of antibiotic resistance threatens our ability to treat common infections, making these crucial drugs less effective over time. By taking your antibiotics exactly as prescribed, not demanding them for viral infections (like colds or flu), and practicing good hygiene, you play a direct role in preserving the power of these life-saving medications for future generations.
These drugs stand as a testament to medical innovation, providing critical solutions for challenging bacterial infections. Knowing their strengths, their applications, and how to use them safely empowers us all to navigate the complexities of modern healthcare with greater confidence and care.