In the ongoing battle against bacterial infections, particularly those caused by stubborn, drug-resistant microbes, third-generation cephalosporins stand as a critical line of defense. These powerful antibiotics represent a significant leap forward in our ability to combat a wide spectrum of bacterial threats, offering enhanced efficacy, especially against challenging Gram-negative pathogens. Their development has been pivotal in managing severe and complicated infections where older antibiotics fall short.
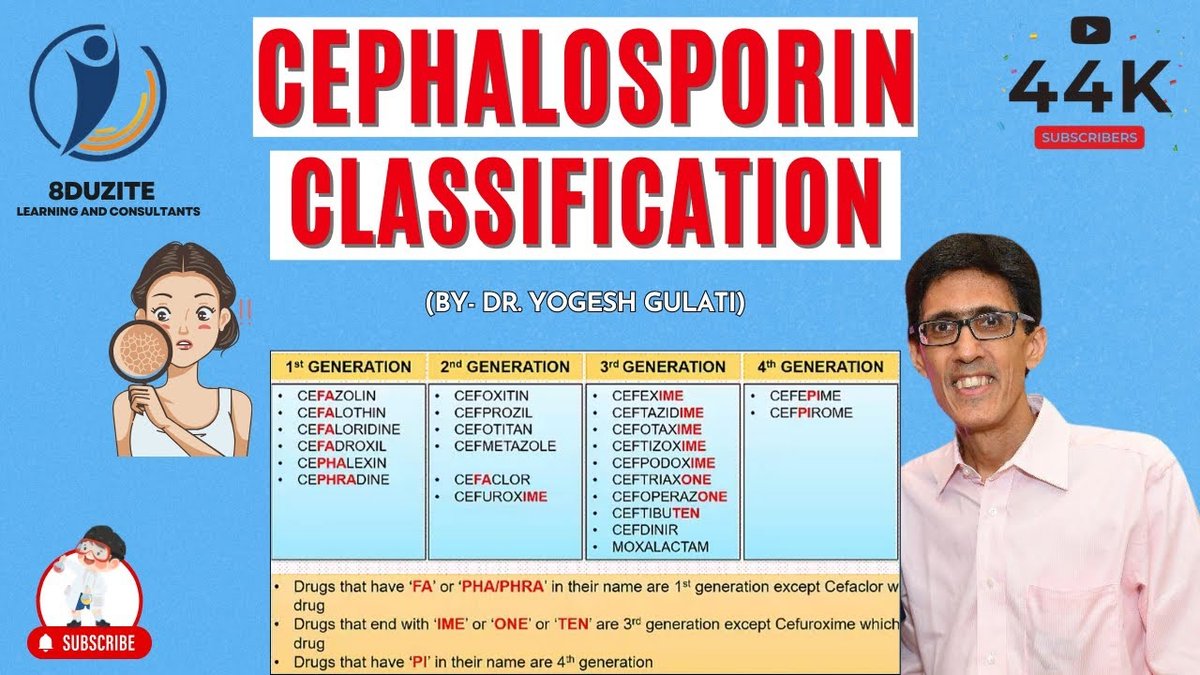
To truly appreciate their impact, it's helpful to understand the broader family of these drugs. Cephalosporins are broad-spectrum, bactericidal antibiotics that derive from the mold Acremonium. They are categorized into five generations, each evolving to tackle different bacterial profiles. For a foundational understanding of this diverse antibiotic class, we invite you to Read our Cephalosporins overview and grasp how these generations have advanced over time.
Unpacking the Potency: How Third-Generation Cephalosporins Work
Third-generation cephalosporins exert their potent effects by targeting the very architecture of bacterial cells. Like their predecessors, they belong to the beta-lactam antibiotic class, meaning they feature a distinctive beta-lactam ring structure central to their action. This ring allows them to bind to and block penicillin-binding proteins (PBPs) within the bacterial cell wall.
By inhibiting these crucial PBPs, third-generation cephalosporins prevent the essential cross-linking of peptidoglycans, a vital step in constructing the bacterial cell wall. Without a properly formed cell wall, the bacteria lose their structural integrity, leading to cell death. This sophisticated mechanism grants them superior activity against Gram-negative bacteria compared to earlier generations, making them invaluable in treating infections resistant to older agents. Delve deeper into the science behind their effectiveness with our comprehensive guide on Mechanism of Action and Antimicrobial.
Diverse Applications: Where Third-Generation Cephalosporins Make a Difference
The versatility of third-generation cephalosporins makes them a cornerstone in treating a broad array of bacterial infections across various body systems. Their enhanced penetration, especially into the central nervous system (CNS) for most agents (excluding cefoperazone, now discontinued), sets them apart. This capability is crucial for severe conditions like meningitis.
Clinicians frequently prescribe these antibiotics for:
- Intra-abdominal Infections: Tackling complex infections within the abdominal cavity.
- Central Nervous System Infections: Including meningitis, due to their ability to cross the blood-brain barrier.
- Skin and Soft Tissue Infections: Managing a range of dermatological and subcutaneous bacterial issues.
- Urinary Tract Infections (UTIs): Especially effective against complicated or resistant UTIs.
- Lower Respiratory Tract Infections: Such as pneumonia and bronchitis.
- Gynecological Infections: Addressing pelvic inflammatory disease and other reproductive tract infections.
- Bone and Joint Infections: Essential for long-term treatment of osteomyelitis and septic arthritis.
- Bacteremia/Septicemia and Sepsis: Critical in life-threatening systemic infections.
Specific agents within this generation also offer unique advantages. For instance, ceftazidime provides excellent antipseudomonal coverage, crucial for infections caused by Pseudomonas aeruginosa. Cefotaxime and ceftizoxime are noted for offering robust Gram-positive coverage among their third-generation peers. Ceftriaxone, with its notably long half-life, allows for convenient once-daily dosing, making it a go-to for conditions like gonorrhea, pelvic inflammatory disease, epididymo-orchitis, and as an alternative for suspected meningitis. To gain a complete picture of their therapeutic reach, Learn Clinical Applications and Indications in our dedicated guide.
Administering Treatment: Dosing and Specific Agents
Third-generation cephalosporins are administered through various routes, including intravenously (IV), intramuscularly (IM), or orally, depending on the specific drug and the severity of the infection. The flexible administration options allow healthcare providers to tailor treatment plans to individual patient needs and infection types. For example, the long half-life of ceftriaxone simplifies patient management by allowing a single daily dose, a significant advantage for both hospital and outpatient settings. Understanding these nuances is crucial for effective treatment; for detailed insights, Understand drug dosing and administration is your next resource.
Some of the widely recognized names in the third-generation cephalosporin family include:
- Cefdinir (Omnicef)
- Cefditoren (Spectracef)
- Cefixime (Suprax)
- Cefotaxime (Claforan)
- Cefpodoxime (Vantin)
- Ceftazidime (Fortaz, Tazicef, Tazidime)
- Ceftazidime/avibactam (Avycaz)
- Ceftibuten (Cedax)
- Ceftizoxime (Cefizox)
- Ceftriaxone (Rocephin)
Each of these agents possesses specific strengths and is indicated for different types of infections, reflecting the nuanced approach required in antimicrobial therapy. To explore the unique characteristics, coverage, and uses of these vital medications, refer to our Key third-generation cephalosporin guide.
Navigating Side Effects and Safety Considerations
While highly effective, third-generation cephalosporins are not without potential side effects. Most individuals tolerate these medications well, experiencing only mild and transient issues. Common side effects can include:
- Abdominal pain and diarrhea
- Nausea and vomiting
- Skin rash and itchy skin
- Inflammation at the injection site
However, more serious side effects can occur, necessitating careful monitoring and patient education. These include: - Hypersensitivity Reactions: Ranging from skin rashes and hives to severe swelling and life-threatening anaphylaxis. It's crucial to note that up to 10% of individuals with a penicillin allergy may also react to cephalosporins.
- Hematologic Issues: Such as leukopenia (decreased white blood cells) and thrombocytopenia (decreased platelets). Drug-induced immune hemolytic anemia (DIIHA) has also been reported.
- Gastrointestinal Complications: The overgrowth of Clostridium difficile can lead to severe pseudomembranous colitis. These antibiotics can also suppress gut flora, potentially reducing vitamin K synthesis and increasing bleeding risk.
- Neurological Effects: Seizures can occur, especially in patients with pre-existing kidney disease.
- Liver Enzyme Elevations: Transient increases in liver enzymes may be observed.
- Disulfiram-like Reactions: Some cephalosporins can cause alcohol intolerance.
- Cardiac Risks: Rapid bolus administration of certain agents, like cefotaxime, has been linked to life-threatening arrhythmias, emphasizing the importance of precise administration as directed by healthcare professionals.
It is paramount that patients communicate any known allergies or adverse reactions to their healthcare provider and adhere strictly to prescribed dosing and administration instructions.
The Future of Fighting Infection
Third-generation cephalosporins remain indispensable tools in the fight against a growing tide of antibiotic resistance, particularly against resistant Gram-negative bacteria. Their broad spectrum of activity, enhanced potency, and ability to penetrate challenging areas like the central nervous system cement their role in modern medicine. As bacterial threats continue to evolve, ongoing research and responsible prescribing practices will ensure these vital antibiotics continue to protect public health for years to come.